The global blood crisis
why medicine urgently needs better alternatives
The world is facing a quiet but serious public‑health crisis: in many regions, there is not enough donated blood to meet medical demand. Even though blood donation is a powerful act of kindness, supply still cannot keep up with rising need.

Blood deserts: when access to blood becomes health inequality
Blood deserts: when access to blood becomes health inequality
Billions of people live in what researchers call “blood deserts” — regions where medical demand for blood is far higher than the amount that can be collected and supplied. This reflects clear inequality in health access:
- Donation imbalance: high‑income countries hold about 16% of the world’s population, but collect roughly 40% of donated blood each year.¹
- Critical regions: countries across sub‑Saharan Africa and South Asia face severe shortages that lead to preventable deaths (postpartum hemorrhage, severe trauma, childhood anemia).²
- Shortages also happen in wealthy countries: the U.S. saw an emergency blood shortage declared in January 2024, with donor levels dropping to the lowest point in about 20 years.³
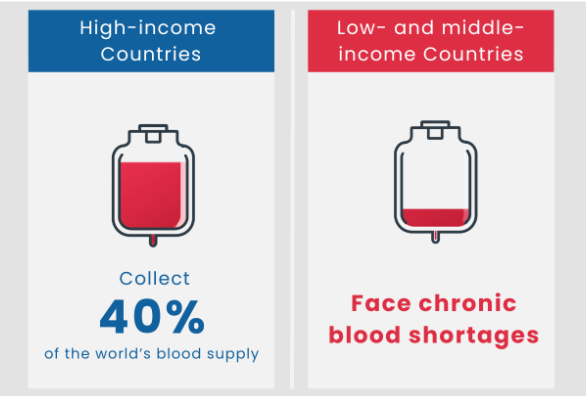
High-income countries (16% of the population) collect 40% of donated blood; most other countries face persistent shortages.
Source: WHO
The hidden risks of donated blood
Shortage is not the only issue. Receiving donated blood (an allogeneic transfusion) also carries risks. Modern screening has made infections like HIV and hepatitis extremely rare, but non‑infectious risks remain important :
- Immune‑related complications: the recipient’s immune system may react to donor components. In some cases this can include transfusion‑related immunomodulation (TRIM), which may increase vulnerability to infection⁴
- TRALI (transfusion‑related acute lung injury): uncommon but a leading direct cause of transfusion‑related death; it can cause acute breathing failure within hours.⁵
- TACO (transfusion‑associated circulatory overload): more common than TRALI, especially in older people or those with heart disease; too much blood too quickly can lead to fluid overload and pulmonary edema.
Beyond infections that can be screened for, what are the real risks that come with receiving someone else’s blood
Because of both global shortages and unavoidable transfusion risks, scientists and clinicians have spent decades developing “artificial blood” or oxygen‑carrying solutions — safer, easier‑to‑use options that could work for everyone in emergencies.
Work cited
-
BMJ Global Health. (2024). Innovative transfusion strategies for blood deserts in disaster settings.
-
Blood DESERT Coalition. (n.d.). The Bleeding Crisis. Retrieved from blooddesertcoalition.org
-
American Red Cross. (2024, January 7). Red Cross declares emergency blood shortage, calls for donations during National Blood Donor Month.
-
Medscape. (n.d.). Immunological Complications of Blood Transfusion.
-
Canadian Blood Services. (2021). Transfusion-related acute lung injury (TRALI). Professional Education.
