The future of artificial blood
From laboratory dreams to hospital reality
The Beginning of the Quest
The pursuit of blood substitutes is not new. It’s a scientific mission that has spanned decades, driven by one simple but vital reason: our current blood donation system has limits. Blood expires within weeks, carries risks of infection, and is often in short supply during emergencies. In times of war, natural disasters, or mass-casualty accidents, the demand for blood often exceeds the available supply. That’s why scientists have long sought the ultimate goal — the “Holy Grail” of transfusion medicine: a blood substitute that is universal, shelf-stable at room temperature, sterile, and ready to use on demand. But this journey has been far from smooth. Early artificial blood projects faced major safety challenges and disappointing results. Today, researchers have shifted focus from creating fully synthetic whole blood toward developing oxygen therapeutics — specialized solutions designed to address specific medical needs
1. Hemoglobin-Based Oxygen Carriers (HBOCs): From Costly Lessons to New Opportunities
HBOCs function by taking hemoglobin — the oxygen-carrying protein — out of red blood cells and allowing it to work freely in circulation. They have clear advantages: long shelf life (over a year), universal compatibility, and the ability to be fully sterilized. However, first-generation HBOCs faced serious side effects
- Vasoconstriction: Free hemoglobin binds nitric oxide, reducing vessel dilation.
- Kidney toxicity: Small molecules filtered through the kidneys cause damage.
- Oxidative stress: Reactive oxygen species injure tissues.
These issues forced several clinical trials — such as PolyHeme® — to end prematurely due to higher-than-expected mortality rates.
Next-Generation Developments
To overcome these problems, researchers adopted new strategies:
- Polymerization – increasing molecular size to prevent leakage (Hemopure®).
- PEGylation – coating molecules to reduce side effects (Hemospan®).
- Encapsulation – enclosing hemoglobin in liposomes to mimic red blood cells.
One of the most promising innovations is M101, derived from the marine worm Arenicola marina. Its hemoglobin molecule is 250 times larger than that of humans, non-toxic to kidneys, and does not cause vasoconstriction.
It has already proven successful in organ preservation, enriching oxygen in tissues before transplantation —a major step toward safer clinical applications.
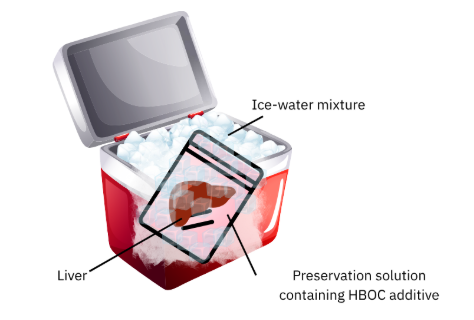
Liver preservation under static cold conditions using an HBOC-enriched solution to pre-oxygenate tissue prior to transplantation.
2. Perfluorocarbons (PFCs): Inert Liquids That Breathe
Unlike hemoglobin, PFCs don’t bind oxygen — they dissolve gases in large quantities. These synthetic compounds must be used as emulsions under high-oxygen conditions to circulate safely in the body. Early products such as Fluosol-DA failed due to side effects and storage issues. However, Perftoran® continues to see limited use in countries like Russia and Mexico, reflecting the variation in global regulatory frameworks.
3. Lab-Grown Red Blood Cells: A Breakthrough from the RESTORE Project
In the UK, the RESTORE Project has pioneered the cultivation of red blood cells from donor stem cells —a process taking about three weeks to produce fully fresh cells. Researchers are now studying whether these lab-grown cells can survive longer in the human body than standard transfused blood. If successful, this could reduce the frequency of transfusions for patients with chronic conditions such as thalassemia or sickle cell disease.
4. Personalized Blood from iPSCs: Australia’s Milestone at MCRI
In 2024, scientists at the Murdoch Children’s Research Institute (MCRI) reached a groundbreaking milestone — creating blood stem cells (HSCs) from a patient’s own tissue using induced pluripotent stem cell (iPSC) technology.
When transplanted into animal models, these cells successfully integrated into bone marrow and produced new blood cells.
This isn’t just about manufacturing bags of blood — it’s about building a “blood factory” inside the body, capable of lifelong blood regeneration. Such an approach could one day cure inherited blood disorders entirely.
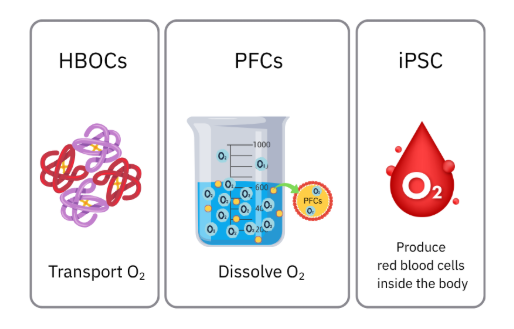
Key mechanisms for replacing or supporting blood function:HBOCs transport oxygen outside red blood cells, PFCs dissolve large amounts of oxygen, and iPSCs generate new blood cells continuously.
Challenges and the Road Ahead
Despite impressive progress, artificial blood technologies still face steep challenges — economic, regulatory, and medical.
The Cost Barrier
Lab-grown blood currently costs up to USD 15,000 per unit,
many times higher than donated blood.
For routine surgeries, that’s unsustainable.
But for patients with chronic transfusion needs — those who require blood every 3–4 weeks for life — the long-term cost of repeated transfusions may actually exceed that of a one-time iPSC-derived stem cell transplant, which could potentially provide a permanent cure.
Regulation and Safety
Each country sets its own approval criteria. Some allow HBOCs in limited applications such as organ preservation or emergency medicine, while others maintain stricter safety thresholds that slow clinical adoption.
Technology as an Ally
Meanwhile, emerging technologies like AI and machine learning are transforming blood management — predicting hospital or regional demand, reducing waste, and improving logistics. Automated blood film image analysis now assists in diagnosing hematologic diseases, ensuring that every drop of donated blood is used more efficiently.
Looking Forward: A Multi-Tech Future
The future of blood security won’t depend on a single winner. It will be a synergy of multiple innovations:
- Smart, AI-optimized blood donation systems
Oxygen carriers for specific emergencies - Lab-grown blood for patients with rare compatibility
- Gene and stem-cell therapies using iPSCs to cure blood disorders at their root
Together, these advancements point toward a world where access to blood is flexible, safe, and reliable — from the operating room to disaster zones.

In the near future, rescue teams equipped with portable artificial-blood technology could deliver oxygen and sustain life from the accident site all the way to the hospital — turning what was once science fiction into a life-saving reality.
Work cited
- Blood Substitutes - ResearchGate, accessed August 6, 2025
- Artificial Oxygen Carriers—Past, Present, and Future—a Review of the Most Innovative and Clinically Relevant Concepts, accessed August 6, 2025
- Blood substitutes- the polyheme trials - PMC, accessed August 6, 2025
- Progress in Development of Functional Biological and Synthetic Blood Products to Augment Transfusable Blood Supply in Operational Medicine, accessed August 6, 2025
- Blood Substitutes: How Close to a Solution? - CancerNetwork, accessed August 6, 2025
- Tracking Research on Hemoglobin-Based Oxygen Carriers: A Scientometric Analysis and In-Depth Review, accessed August 6, 2025
- LETTER TO EDITOR MARINE RESOURCES: POTENTIAL OF POLYCHAETE APPLICATION IN COMBATING COVID-19 INFECTION - JSSM, accessed August 6, 2025
- Complement-Mediated Acute Effects of Liposome-Encapsulated Hemoglobin, accessed August 6, 2025
- marine resources: potential of polychaete application in combating covid-19 infection, accessed August 6, 2025
- World-First Trial Transfusing Lab-Grown Red Blood Cells Begins, accessed August 6, 2025
- Blood stem cell breakthrough could transform bone marrow transplants - Murdoch Children's Research Institute, accessed August 6, 2025
- Lab-developed blood stem cell success in Australia - British Society for Haematology, accessed August 6, 2025
- reNEW researchers lead world-first blood stem cell breakthrough, accessed August 6, 2025
- Blood stem cell breakthrough could transform bone marrow transplants - University of Birmingham, accessed August 6, 2025
- Lab-grown blood stem cells - News - Nature Middle East, accessed August 6, 2025
- Development of blood demand prediction model using artificial intelligence based on national public big data, accessed August 6, 2025
- From microscope to micropixels: A rapid review of artificial intelligence for the peripheral blood film - PubMed, accessed August 6, 2025
- Artificial intelligence for the detection of acute myeloid leukemia from microscopic blood images; a systematic review and meta-analysis - PubMed, accessed August 6, 2025
- Machine learning in transfusion medicine: A scoping review - PMC, accessed August 6, 2025
